This prevalent issue is frequently overlooked or misinterpreted. Pelvic organ prolapse, a disease in which the uterus, bladder, small intestine, or rectum bulges into the vaginal wall or drops down through the vagina, affects around half of the women over 50. However, unlike other prevalent health issues, many women are reluctant to discuss it, even with their doctors. Some people do it out of embarrassment, while others do it because they believe it's simply something they'll have to cope with as they get older.
Pelvic organ prolapse conditions
Normal positions of pelvic organs

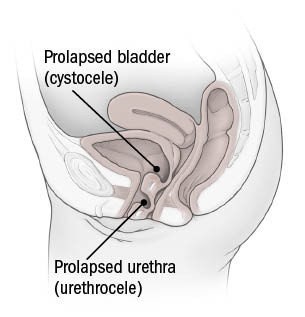
Cystocele and urethrocele
Rectocele

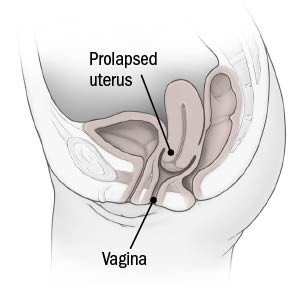
Uterine prolapse
The topic of whether having the COVID-19 vaccination might impact my mammography findings was raised in an article authored by Kelly Bilodeau, Executive Editor, Harvard Women's Health Watch.
He explained that as your immune system prepares to detect and fight the virus, at least two of the authorized COVID-19 vaccinations may cause lymph nodes in the armpit (or other parts of the body) to swell. Although it's a safe transient response, it might cause some confusion on a mammogram. Swollen lymph nodes in the armpit or other surrounding areas are an indication of cancer in rare situations. Experts are now urging radiologists to use caution when interpreting the importance of enlarged lymph nodes observed on a woman's mammography if she has recently received the COVID-19 vaccination, to prevent unneeded testing and worry. If your breast imaging centre hasn't inquired about it, please do so. If your mammography reveals enlarged lymph nodes, your radiologist may recommend that you have further ultrasound testing or return in a few weeks to check if the swelling has subsided. If the swelling does not go away, further testing may be required. To minimize problems, schedule your mammogram before your first dosage or four to six weeks after your second dose. But don't forget to take the test and get your COVID-19 vaccine.
Browsing through venues is one of the most lust-worthy portions of the wedding planning process, right up there with engagement rings and bridal dresses. However, with so many options—at every price point— but it may be difficult especially if you aren't sure where you want to marry. Inspiration and direction are required even for the most imaginative bride.
Your wedding location, which is the most essential aspect of any wedding, makes the celebration spectacular. With years-long waitlists for the most sought-after destinations, it's important to prepare ahead, especially for the most awe-inspiration. Because the location you choose will appear in every image and memory from the day, it's critical to select a location that reflects the significance of the wedding, stunning all guests with its uniqueness.
Here are our top selections for the most beautiful wedding venues across the world, ranging from European chateaux to tropical beaches and unusual American locations.
Your baby has come after 40 weeks of doctor appointments, nursery preparation, and anticipation. You think she's wonderful, healthy, and cute. Over the next few weeks, your excitement is replaced with anxiety: Is she eating enough? Whoa, why does she cry? Is she ill? These concerns follow you around all day and night. You're right, irritated, and anxious. Your loved ones start to worry about you, not just the baby. You wonder if your stress is typical.
Baby blues, ptd, or pta? (postpartum depression, or postpartum anxiety).
You've probably heard of baby blues or postpartum depression. During your postpartum medical appointment, you may have been asked about your mood. Hormone levels drop after birth, causing feelings of sadness, weeping, and overwhelm. These symptoms are minor and only last a few weeks. It's possible that something else is causing the symptoms.
Symptoms of PPD and anxiety (such as poor sleep, trouble relaxing, and irritability). Some women have prenatal and postnatal anxiety, but only a small percentage of those parents experience postpartum depression. Postpartum depression can make it challenging for women to respond to treatments like interpersonal psychotherapy or prescription antidepressants like bupropion (Wellbutrin).
Momentary bouts of postpartum anxiety, like with postpartum depression, might be related to hormone fluctuations. It may also rise in reaction to actual pressures, such as the baby's health, money, or negotiating new responsibilities in relationships. If a woman has experienced pregnancy loss (miscarriage or stillbirth) this can enhance her chances of having postpartum anxiety. Anxiety symptoms may recur after birth if you had anxiety before or during pregnancy. Hormonal changes can cause anxiety and sadness after weaning.
Postpartum panic episodes or OCD symptoms are common. Fear, dread, panic, shortness of breath, and dizziness are among the signs of panic attacks. Unwanted thoughts and compulsions, or deliberate actions to ease discomfort, are called obsessions. Unsettling symptoms for new mothers, especially when they entail hurting the child. Fortunately, obsessions caused by anxiety disorders seldom cause harm to newborns.
Even if your overall body weight is within acceptable limits, extra belly fat increases your risk of heart disease, according to the American Heart Association (AHA) in a statement published online by Circulation on April 22, 2021. The most dangerous form of fat for your heart, according to the AHA's evaluation of the research, is visceral adipose tissue (VAT), which is found deep within your body, surrounding your organs. not the type of fat that you can touch just beneath the skin. VAT is a physiologically active chemical that produces inflammatory molecules that can damage blood vessels and create other cardiovascular issues.



